
Tirotta D 1, Lena C 1., Del Prete V 1, Gardelli L 1., Tassinari M 1., Compagnone M 2., Galvani M 2., Muratori P 1
1Department of Internal Medicine, Cervesi Hospital, Cattolica, (RN), AUSL Romagna, Cattolica, Italy.
2Cardiology Unit Morgagni Pierantoni Hospital, Forlì
*Corresponding author: Tirotta D, From the Department of Internal Medicine, Cervesi Hospital, Cattolica, (RN), AUSL Romagna, Cattolica, Italy.
Received: March 27, 2023
Accepted: April 21, 2023
Published: May 20, 2023
Citation: Tirotta D, Lena C., Del Prete V, Gardelli L., Tassinari M., Compagnone M., Galvani M., Muratori P. (2022) “Respiratory Failure, Previous Stroke and Pulmonary Embolism: Mind The Platypnea- Orthodeoxia Syndrome.” J Clinical Cardiology Interventions, 3(1); DOI: http;//doi.org/10.2022/1.1033.
Copyright: © 2023 Tirotta D. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Platypnea-orthodexia syndrome (POS) is an unusual presentation of several pathologies.
The exact prevalence of this syndrome remains, however, unknown. Despite this, many diseases are associated with POS, which is increasingly identified by clinicians.
The pathophysiological mechanism associated with this syndrome is not yet fully understood, but probably results from one of the following : intracardiac shunt, pulmonary shunt, ventilation-perfusion mismatch or a combination of these three mechanisms
Although the underlying disease of POS may be present from the birth, symptoms may appear only later in life due to an acute superimposed illness.
It is necessary to mind the POS in the presence of an unexplained dyspnea or a dyspnea associated with cardioembolic manifestations and /or venous embolism in anamnesis. The presence of both arterial and venous Thrombophilic diathesis makes the differential diagnosis with an antiphospholipid syndrome, while the association of stroke and dyspnea, with aspiration pneumonia.
We introduce a case of POS with a past pathological history of embolic stroke and pulmonary embolism and we carry out a sensible literature review of POS cases associated to this presentation
Background
(POS) is an unusual presentation of several pathologies.
Platypnea means development of dyspnea in the upright position (sitting or standing position). It is, therefore, a postural dyspnea, also recorded in the right lateral position. Orthodeoxia, on the other hand, refers to hypoxemia triggered by the same postural change.
There is no consensus of an accurate cut-off for arterial oxygen desaturation, generally identified as a decrease in PaO2 > 4 mmHg and of SaO2 > 5%.
Usually, the severity of hypoxemia is mild; some patients experience severe reduction in PaO2. (1)
Reports in the literature show that patients with POS have other adjunctive symptoms, such as nausea, tachycardia, tachypnea, drop in systolic blood pressure when in upright position (1-23)
A sensitive search on PubMed shows more than 200 cases of POS recorded. The exact prevalence of this syndrome remains, however, unknown. Despite this, many diseases are associated with POS, which is increasingly identified by clinicians.
The pathophysiological mechanism associated with this syndrome is not yet fully understood, but probably results from one of the following : intracardiac shunt, pulmonary shunt, ventilation-perfusion mismatch or a combination of these three mechanisms (Tab 1). (1)
In the majority of cases the structural anomaly underlying the POS is an intracardiac shunt: Patent Foramen Ovale (PFO), Atrial septal defect (ASD), atrial septal aneurysm (ASA). The intracardiac mechanism is present in > 80% of patients with POS.
Another functional aberration is the intrapulmonary shunt or the Ventilation perfusion mismatch (Zone 1 phenomenon): there is a physiological inequality in the distribution of perfusion in a normal lung. Blood flow and intravascular pressure increase, resulting in a pressure gradient of approximately 23 mmHg. This difference is gravitationally determined by the interactions between alveolar, arterial, and venous pressures. In Zone 1, located in the apical region, blood flow is present only during systole, because the alveolar pressure is higher than the arterial and venous pressures. In Zone 2, where Pa is > alveolar Pa and flow is nearly continuous. In Zone 3, arterial pressure dominates over venous and alveolar pressures and blood flow is constant. As gravity is the most crucial thing in lung perfusion heterogeneity, supine decubitus almost abolishes these differences, and virtually, the entire lung behaves like Zone 3. In this way, postural change from lying to sitting or standing increases flow only to the lower lung regions (1)
Although the underlying disease of POS may be present from the birth, symptoms may appear only later in life due to an acute superimposed illness.
It is necessary to mind the POS in the presence of an unexplained dyspnea or a dyspnea associated with cardioembolic manifestations (2-19) and /or venous embolism in anamnesis. The presence of both arterial and venous Thrombophilic diathesis makes the differential diagnosis with an antiphospholipid syndrome, while the association of stroke and dyspnea, with aspiration pneumonia.
We introduce a case of POS with a past pathological history of embolic stroke and pulmonary embolism and we carry out a sensible literature review of POS cases associated to this presentation.
Method
We introduce a case report and a review of Platypnea-orthodexia syndrome cases published in the literature in the last 10 years.
We performed a sensible research on PubMed (Keywords “Platypnea-orthodexia syndrome” “pulmonary and embolism” and “stroke”), with control of references.
We obtained 4 cases (20-23); (temporal limits: 2010–2020), age limit (adult: 19+ years), and language limit (English language) (Table 2).
RESULTS
Results: our case and literature review
Epidemiology
Our patient is a 89-year-old female.
Literature review
In our series, the main age of presentation of the syndrome, in patients with a history of stroke and pulmonary embolism, is 76.2 (67-89 years). There is no gender prevalence.
Clinical Picture
Our case: chronic respiratory failure and recurring hospital admission for this clinical problem: after a week from last hospitalization, the patient enters to our hospital Unit for dyspnea in orthostatism, fever (respiratory rate 16 breaths per minute, Tc 37.8 C, Pa 120/60 mm Hg, SaO2 89%)
Chest Rx Ray showed minimal pleural effusion. Hight resolution computed Tomography (HRCT) showed consolidation areas in posterior basal area; small areas of ground-glass more evident in the posterior regions. Minimal pleural effusion. Gross hiatal hernia. Enlarged heart. Dilatation of the aorta ascending thoracic with diameter up to 4.5cm (Fig 1).
Literature review
Patients suffer from dyspnea and/or hypoxemia both in the upright and in the sitting position. These symptoms are attenuated or disappear within a few minutes by assuming a supine position. The patients do not respond to traditional therapies for chronic lung disease, left ventricular dysfunction or coronary artery disease and the cause of the worsening dyspnea is not understood, even if using the objective method of problem solving.
Physiopathology
Our case
Patent Foramen Ovale (PFO) associated with some functional aberrations as hiatal hernia, dorsal kyphoscoliosis, ascending aortic ectasia, recent bilateral pneumonia, previous paucisymptomatic Covid 19 infection (Fig 2).
Literature review
In most cases (4/5) the structural anomaly underlying the POS is an intracardiac shunt. In a minority of cases the structural alteration is an intrapulmonary shunt: pulmonary arterio-venous malformation.
Actually, the interaction of multiple structural and physiological alterations is necessary to develop a POS, given the high prevalence of PFO in the general population (about 25-30% depending on age) and the low prevalence of this syndrome in the general population.
In a minority of cases (2/5) the functional aberration occurs in the presence of a normal right atrial pressure, due to an intrathoracic extracardiac anomaly (Hiatal hernia, dorsal kyphoscoliosis, recent bilateral pneumonia, diaphragmatic paralysis) or cardiac (ascending aortic ectasia) anomaly.
In other cases, on the other hand, an increased pressure in the right atrium occurs (for example due to a pulmonary embolism).
The gravitational effects of upright posture change the intracardiac relationship of structures with an alignment of blood flow, from the inferior vena cava and the interatrial septum.
Another functional aberration is the Intrapulmonary shunt.
Diagnostic assessment
Our patient
Echocardiography showed mild left ventricular hypertrophy with normal ejection fraction; left atrium was imprinted by extracardiac mass
(hiatal hernia); aortic aneurysm ascending.
Transcranial color Doppler showed right-left shunt of significant degree (SPENCER=5).
Finally Transesophageal cardiac eco color Doppler showed an oval fossa with large mobile aneurysm and long tunnel (10mm). Large basal shunt.
Bubble test is performed before and after applying the device (Fig 3).
Literature review
Transesophageal echocardiography is decisive in the diagnosis of cardiac shunt, and it should be done as a last step if Transcranial color Doppler is positive. CT angiography in pulmonary arteriovenous malformations (AVMs)
Treatment
Our patient underwent to PFO percutaneous closure with a specific device. As a result of the procedure, remarkable and immediate improvement of peripheral saturation in a few minutes (SpO2 93% in orthostatism) occurred.
In relation to the presence of paroxysmal atrial fibrillation and to the recent closure of the PFO, direct oral anticoagulant therapy was started.
Literature review
In all cases after the therapeutic intervention there was a fast clinical remission
Conclusion
The analysis of our case and the literature review show that:
The presence of a worsening dyspnea not etiologically explained and not responsive to the usual therapies, must make us think of a possible POS among the diagnostic hypotheses, even if this syndrome is unusual. It is recommended to mind the POS in problem solving to avoid cognitive bias.
It is important to remember to keep in mind a POS in the presence of typical symptoms of respiratory failure associated with cardioembolic manifestations and/or arterial and venous thrombosis together. Paradoxical embolism is a rare entity due to occurrence of a venous thrombotic event associated with a systemic arterial embolism.
Patients with pulmonary embolism have worse outcomes in the presence of a PFO due to risk of paradoxical embolization. Physicians should be cognizant of embolization in different vascular beds.
It is not unusual for PFO associated with shunts to manifest in adulthood due to functional aberrations that arise over time (aneurysm of the ascending aorta, hiatal hernia, kyphoscoliosis, covid-related pneumonia)
Cardioembolic stroke and POS are two sides of the same coin for secondary shunting to a PFO. Correction of stroke-associated Foramen Ovale must, however, be more rigorous than in POS.
PFO closure is a low-risk procedure that promptly resolves hypoxia and reduces a future risk of paradoxical embolization. An early diagnosis of POS is important, since the intervention of the shunt, cardiac or pulmonary, generally resolves the clinical picture in a short period of time.
Given the effectiveness of shunt correction, it should also be done also in the elderly people
|
INTRACARDIAC SHUNT PLATYPNEA ORTHODEOXIA SYNDROME
1a) In the setting of normal right atrial pressure, INTRINSIC CARDIAC ANATHOMICAL PATOLOGY
1b) In the setting of normal right atrial pressure and EXTRACARDIAC INTHRATORACIC PATHOLOGY
EXTRACARDIAC (PULMONARY) SHUNT
MISCELLANEOUS MECHANISMS Parkinson’s disease Diabetic autonomic neuropathy Amiodarone lung toxicity |
Table 1: Main causes of POS (1, modified)
|
|
Our case |
Constellation of Stroke, Pulmonary Embolism, and Platypnea-orthodeoxia syndrome. The Elusive Patent Foramen Ovale. 2021
|
Platypnea-orthodeoxia syndrome after recent stroke: a case report of a sandwiched right atrium 2022 |
Stroke and Respiratory Failure: Mind the Shunt! 2021
|
A case report of platypnea-orthodeoxia syndrome: an interplay of pressure and blood flow 2019
|
|
Age, gender
|
89 years, female |
67-year-old male |
71-year-old male |
74-year-old female |
80-year-old female |
|
Comorbidity |
- Hypertension, paroxysmal atrial fibrillation in warfarin, Hypercholesterolemia, Previous ischemic stroke (2001) with probable cardioembolic origin
-PREVIOUS ADMISSION -in Geriatric Unit due to subjective dizziness, finding of pulmonary embolism - in Internal medicine Unit (2 months ago) for respiratory failure due to congestive heart failure and bilateral pneumonia - in Internal Medicine Unit (1 month ago) due to congestive heart failure |
Not specified |
Medical history of recent stroke |
Previous history of cerebrovascular disease and recurrent episodes of spontaneous epistaxis |
Not specified |
|
Baseline abnormality
|
Patent Foramen Ovale (PFO) |
SIA (aneurysm) associated with shunt
|
Patent Foramen Ovale (PFO) |
3 pulmonary arterio-venous malformation
(PAVM) |
Patent Foramen Ovale (PFO) |
|
Actual triggering anomaly
|
Hiatal hernia, dorsal kyphoscoliosis, ascending aortic ectasia, recent bilateral pneumonia, 7 months before paucisymptomatic Covid 19 infection
|
Pulmonary embolism, diaphragmatic paralysis
|
Root of the aorta dilated and elevation of the right hemidiaphragm. Right atrium compressed between the two structures (sandwiched) |
Pulmonary embolism |
Pulmonary embolism |
|
Timing of clinical events
|
Previous stroke and pulmonary embolism (years ago), previous admission for respiratory failure
|
After prostatic surgery> POS> stroke
|
Recent stroke. Hospitalization for respiratory failure
|
History of stroke>> hospitalization for stroke dysarthria>> Respiratory failure and POS |
|
|
Diagnostic tests |
. - Echocardiography: mild left ventricular hypertrophy with normal ejection fraction; left atrium imprinted by extracardiac mass (hiatal hernia); mitral and aortic valve sclerosis; aortic aneurysm ascending
. - Transcranial color Doppler: right-left shunt of significant degree (SPENCER=5).
- Transesophageal cardiac echo color doppler : oval fossa with large mobile aneurysm and long tunnel (10mm). Large basal shunt. Mitral and aortic degenerative disease. Mild aortic regurgitation and minimal mitral valve regurgitation |
-Transthoracic echocardiography demonstrated an aneurysmal interatrial septum and a mildly positive bubble study within 3 heartbeats suggestive of a right-to-left shunt (RLS) at the atrial level.
-During cardiac catheterization, the mean right atrial pressure was 8 mm Hg with a mean left atrial (LA) pressure of 11 mm Hg. -Transesophageal echocardiography confirmed a Patent Foramen Ovale (PFO).
|
-A contrast computed tomography excluded pulmonary embolism and revealed a dilated aortic root and an elevated right hemidiaphragm.
-A transesophageal echocardiography confirmed the presence of a persistent Patent Foramen Ovale (PFO) in supine position. In upright position, there was a torrential increase in right-to-left shunting. |
-A transthoracic echocardiogram did not show an intracardiac shunt.
-The computed tomography (CT) pulmonary angiogram revealed pulmonary thromboembolism and 3 large pulmonary arteriovenous malformations (PAVMs) in the left pulmonary field |
-Angio-CT scan of lungs showed no signs of PE
-The ventilation/perfusion scan showed several small peripheral emboli in the pulmonary vascular bed. -In another TTE, no significant changes were identified. -A transesophageal echocardiography showed an interatrial septum with an exuberant hyperdynamic movement, with abundant passage of contrast from the right atrium to the left, even without performing the Valsalva manoeuvre, compatible with an important PFO |
|
Clinical Evolution |
• Persistence of respiratory failure with need of ventilatory support e orthostatic desaturation associated with dyspnea.
• Orthostasis: • EGA RESERVOIR 15 L/min: • pH 7.54, pO2 39, pCO2 28.5, sO2 78% • EGA AIRVO FiO2 90% + RESERVOIR 15 L/min: pH 7.5, pO2 40, pCO2 25, HCO3- 21, SpO2 79%
• Lying: • EGA AIRVO FiO2 90% + RESERVOIR 15 L/min: • pH 7.5, pO2 70, pCO2 28.3, SpO2 95% |
He required intubation for hypoxemia ([SaO2] = 62%) that only partially responded to high-flow oxygen; he was extubated after 24 h when his hypoxemia resolved while supine. |
During observation in the emergency department, desaturation was noted in upright position.
.
|
Progression to respiratory failure and need for invasive mechanical ventilation. After endotracheal intubation, the oxygen saturation improved |
PH supine: 7.44, 45 ° 7.41, sitting: 7.43
PCO2 supine (mm Hg): 30.8 , 45 ° 32.8, sitting: 32.9
PO2 supine (mm Hg): 76.7 , 45 ° 40.2, sitting: 52.5
SO2% supine: 96.9% , 45 ° 77, sitting: 88.5
|
|
Initial therapy |
|
Not specified |
Not specified |
Not specified |
Not specified |
|
Therapy and post therapy evolution
|
The patient underwent to percutaneous closure surgery of the PFO with device. Bubble test is performed before and after applying the device. As a result of the procedure, remarkable e immediate improvement of peripheral saturation in a few minutes (SpO2 93% in orthostatism). In relation to the presence of paroxysmal atrial fibrillation and to recent closure of the Foramen Ovale Patent. |
SaO2 normalization a few minutes after PFO closure
|
Directly after the procedure of PFO closure, the patient was symptom free |
Endovascular embolization of the PAVMs was performed and there was a progressive increase in oxygen saturation from 85 to 99% at the end of the procedure. The patient was successfully extubated 2 days after the procedure |
|
Table 2: Our case and literature review of POS Syndrome associated with stroke and pulmonary embolism
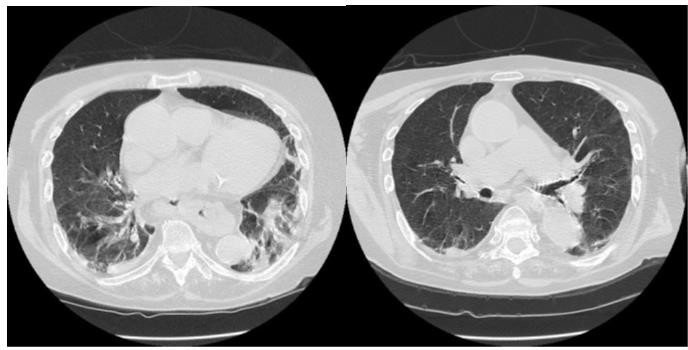
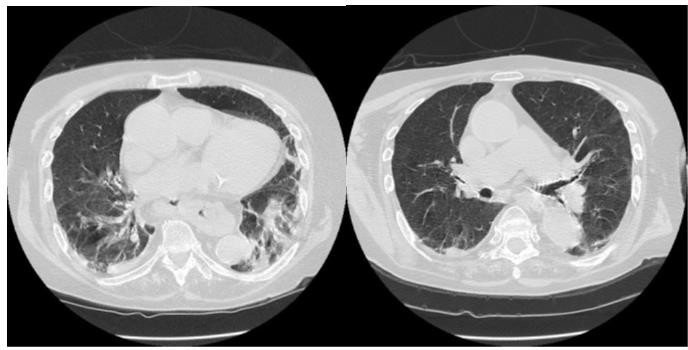
Figure 1: HRCT and chest X ray of our patient
Figure 2: Cause and functional aberrations of POS in our patient
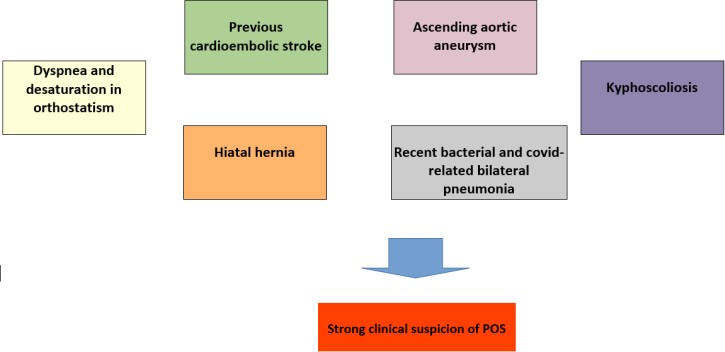
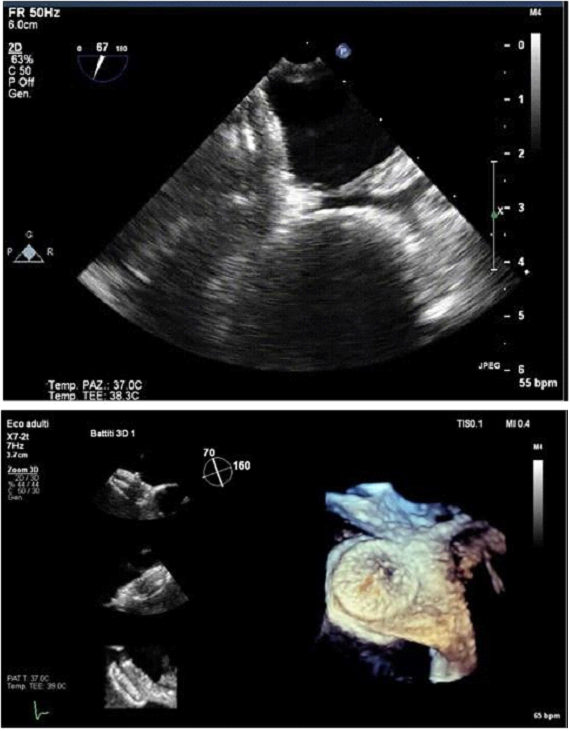
Figure 3: Bubble test before and after the device